Free vaccination against cervical cancer is currently ongoing in 16 states of the federation, including the Federal Capital Territory (FCT). Unfortunately, the programme in some states is threatened by several challenges such as fake news that the jab is a conspiracy from the West to reduce the fertility of Nigerian women, corrupt practices, unnecessary delays and out-of-stock syndrome. However, several local and international studies have endorsed the jab to be safe and 99 per cent effective in preventing cervical cancer, writes MUSA ADEKUNLE.
The plan by the Federal Government to immunise teenage girls against cervical cancer with Human Papillomavirus Vaccine (HPV) is facing daunting challenges, as there is vaccine hesitancy or outright rejection by some parents due to fears that the jab is associated with contraception/family planning.
The Guardian investigations revealed that some centres charge fees for the vaccine, which is supposed to be free, while some others easily run out of stock; and making patients wait for longer hours, days and even weeks to get vaccinated.
Indeed, since the introduction of the free dosage of the HPV vaccine into Nigeria’s routine immunisation system, in October 2023, the vaccination exercise has been inundated by a deluge of misinformation and misconceptions, leading to the hesitancy of some people to take the vaccine.
The first phase of the planned nationwide rollout covers 16 states including Abia, Adamawa, Akwa Ibom, Anambra, Bauchi, Bayelsa, Benue, Enugu, Jigawa, Kano, Lagos, Nasarawa, Ogun, Osun, Taraba and the Federal Capital Territory (FCT).
According to the government, about 7.7 million girls are targeted for the free dosage. Though the vaccination programme has been going on since October at different primary healthcare centres across the country, however, some misconceptions about the vaccine are preventing many people from participating in the programme, similar to what was seen during the COVID-19 vaccination.
There are claims that the West is using the HPV vaccine to reduce the population of Africa, the vaccine is a way to inject HIV into the bodies of young girls so that they could die in the future, and that Nigerian leaders have been sponsored to give up their country to their enemies.
These claims, which are shared on different social media platforms, especially WhatsApp in northern Nigeria, where audio recordings in Hausa are forwarded widely to individuals and groups are causing mass confusion and instilling fear in people.
There’s no evidence to support the claim that the HPV vaccine was introduced to control the population in Nigeria. This is a common myth spread in relation to most other vaccines introduced in the country. The polio and COVID vaccines were also accused of causing infertility, but many of those who took the shot have given birth and continued to be fertile.
Prof Akinyinka Omigbodun of Obstetrics and Gynaecology Department, College of Medicine, University of Ibadan told The Guardian, said that the fight against cervical cancer has been a tortuous one with unexpected turns, recalling that the first notable observation was to suggest that cervical cancer is sexually transmitted and its rarity among nuns in the 19th Century.
According to him, it took more than one hundred years after that before it was proved that the human papilloma virus (HPV) was responsible for more than 99 per cent of all cervical cancers. The next logical step was to find out if the prevention of HPV infection will lead to prevention of cervical intraepithelial lesions (CIN), the precursors of cervical cancers.
The successful preparation of effective vaccines against the most common strains of HPV about 30 years ago made that type of research feasible. The outcome far exceeded scientists’ expectations. More than 95 per cent of pre-adolescent girls and boys who were vaccinated did not have detectable HPV infection in the subsequent years and practically none of the girls developed CIN.
According to him, “Calling HPV vaccine a game changer does not sufficiently describe its impact on reproductive health, it has made cervical cancer the first highly prevalent cancer that can be prevented by vaccination, and that has been the experience everywhere it has been introduced.
“Its introduction in Nigeria is something that Gynaecological Oncologists (those of us who specialise in the care of cancers of the female reproductive tract) have been looking forward to. We expect that once more than 70 per cent of all adolescent girls are vaccinated in the country; we can prevent more than 90 per cent of the approximately 12,000 cervical cancers that are diagnosed in Nigerian women every year. That will mean preventing the deaths of nearly 8,000 Nigerian women in the most productive years of their lives. That is more than a “game-changer”, it is a lifeline to Nigerian women,” he added.
Speaking on insinuations that the jab is a conspiracy from the West to reduce fertility of Nigerian women, corrupt practice, Omigbodun, who is Past President, West African College of Surgeons (WACS) stated that there is always a gap between the stage where scientists prove that a particular intervention is effective in solving a public health problem and when such measures are effectively implemented for the benefit of the public.
He said: “There are always obstacles to public health measures from the human factor. That is why the effective deployment of public health measure cannot be left to scientists or doctors, nurses and other healthcare providers alone; we need to involve those in the humanities (sociologists, and anthropologists), community leaders and opinion leaders, including those who make the most effective use of social and mass media.
“The HPV vaccine will not be the first to face challenges before its wide acceptance and application. Such challenges were overcome with smallpox vaccination in the 1960s, and more recently, with polio vaccination among infants and under-fives in Nigeria. They will also be overcome with HPV vaccination. The myths and unfounded rumours are many, the most pernicious being that HPV vaccination would make the youth more sexually promiscuous or it could lead to infertility. Research done in other places has shown clearly that this is not the case.
“Some of the research we have done here demonstrates very clearly that, with proper health education, young school girls and their parents are very willing to accept HPV vaccination. As for corrupt practices, that is something the health authorities, the Federal Ministry of Health and Social Welfare, the National Primary Healthcare Agency and the State ministries of Health, will need to provide effective field supervision to ensure that such corrupt practices do not take root or impede the rollout of the vaccination.”
The vaccine has also been approved by WHO and the National Agency for Food and Drug Administration and Control (NAFDAC) for use in Nigeria. Both the Nigeria Centre for Disease Control (NCDC) and WHO have certified the HPV vaccine as safe. It has been tested not only in Nigeria but in many other countries across the world. People in countries such as the United States, Brazil, and China have all received the vaccine.
According to a study titled, ‘Spotlight on Human Papillomavirus Vaccination Coverage: Is Nigeria Making Any Progress?’ published in the journal JCO Global Oncology, moving forward, if Nigeria is to make considerable progress in fully immunising the estimated 15 million Nigerian girls aged nine-14 years, the country must be deliberate in leveraging every opportunity that puts them in a good position to sustainably roll out HPV vaccines nationally.
The success of the HPV vaccine rollout in Rwanda since 2011 which put the country on a path toward the elimination of cervical cancer after high HPV vaccine coverage (92.23 per cent) of the target population serves as a key example of what strong political commitment, government ownership, and leadership can accomplish.
As Nigeria begins to roll out HPV vaccination, it is equally important to establish strong accountability mechanisms including robust monitoring and evaluation frameworks that highlight progress, identify multilevel challenges across the HPV vaccine introduction process, and proffer solutions to improve programmes operations and sustainability.
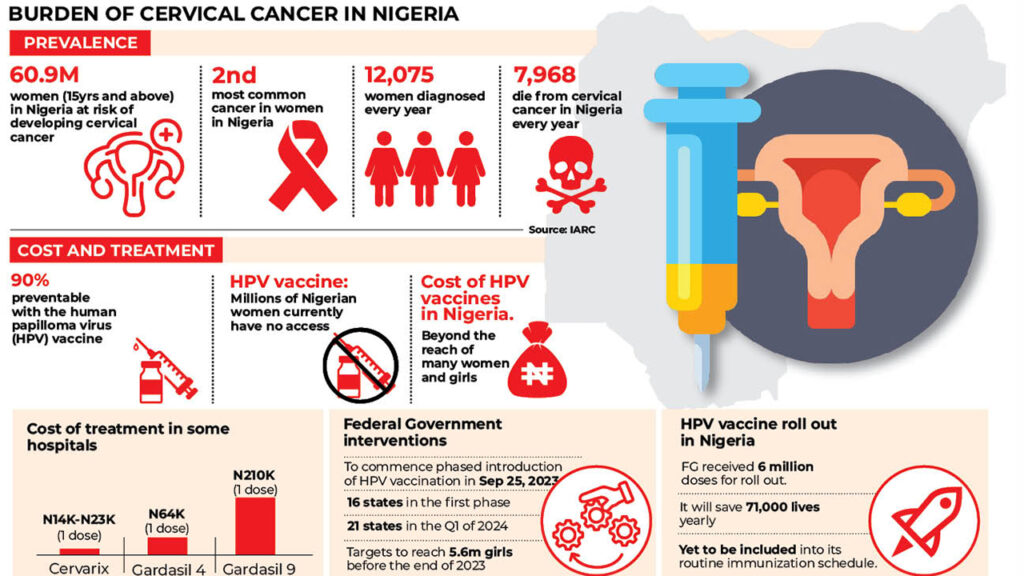
According to the researchers, the tragedy of losing one woman every two minutes to cervical cancer is regrettable in the face of advancements in cervical cancer prevention and treatment. Despite being a largely preventable disease through HPV vaccination and screening, the burden of cervical cancer is increasing each year with a concomitant widening of global health inequities. In terms of global cancer incidence and mortality, cervical cancer ranks fourth with an estimated 604,000 new patients and 342,000 deaths in 2020.
It is alarming to note that about 90 per cent of the global cervical cancer incidence and mortality occur in low- and middle-income countries (LMICs), with women of low socioeconomic status bearing the greatest burden. Such disparities in cervical cancer burden demonstrate huge socioeconomic gaps between countries and inequitable implementation of cervical cancer prevention and control measures including HPV vaccination and organized screening programmes. Hence, it becomes morally imperative to address stark inequities in global cervical cancer burden and prevention efforts especially in LMICs.
In Nigeria, an estimated 12,000 cases and 8,000 deaths in 2020 puts cervical cancer as the second leading cause of female cancer morbidity and mortality behind breast cancer. The 90-70-90 targets to be met by 2030 as contained in the global strategy to accelerate the elimination of cervical cancer as a public health problem raises optimism among LMICs including Nigeria despite skeptics describing it as overly ambitious and unrealistic.
Specifically, the 90-70-90 targets set out to see that 90 per cent of girls are fully vaccinated with HPV vaccine by age 15 years, 70 per cent of women are screened with a high-performance test at 35 years and again at 45 years and that 90 per cent of women identified with cervical disease receive treatment.
Vaccination of adolescent girls with HPV vaccines before the onset of sexual activity is the most effective long-term intervention for reducing the risk of developing cervical cancer. Knowledge of the causal relationship between HPV infection and cervical cancer has stimulated advances in the development, licensing, and usage of HPV vaccines. Evidence from population studies including post-vaccination follow-up has shown HPV vaccines to be highly immunogenic, safe, and effective in preventing HPV infection, cervical lesions, anogenital warts, and other HPV-related diseases.
Currently, six HPV vaccines are licensed for use by the WHO – bivalent HPV vaccines (cervarix, cecolin, and walrinvax), quadrivalent HPV vaccines (gardasil and cervarix), and nonavalent HPV vaccine (gardasil9). Providing protection against high-risk (oncogenic) HPV types 16 and 18 that cause the majority of precancers, cervical cancers, and other HPV-related cancers is a unique characteristic across the licensed vaccines.
WHO’s guidelines recommend that adolescent girls between nine and 14 years receive two doses of vaccine to be fully immunised with at least a six-month interval between doses, with exceptions for special populations including immune-compromised individuals and those age 15 years or older, for whom three doses are recommended.
The National Agency for Food and Drug Administration and Control (NAFDAC) approved the use of the Gardasil vaccine as a single dose in the routine immunisation against cervical cancer. In 2022, following evidence that a single dose of HPV vaccine provided similar protection against HPV infection as seen in multi-dose regime, the WHO updated its HPV vaccination recommendations to include a single-dose schedule (also referred to as alternative or off-label single-dose schedule) for individuals aged nine-20 years. The single-dose schedule update is timely and can help countries such as Nigeria to introduce the HPV vaccine, improve coverage, and cut associated costs.
Financial and programmatic barriers including high vaccine cost, lack of political will, vaccine logistics challenges, health workforce gaps, and global HPV vaccine supply constraints have been adduced as major reasons for inequitable national introduction of HPV vaccination especially in LMICs where vaccines are needed the most.
The interventions of Gavi, The Vaccine Alliance – a global public-private partnership targeted at addressing major precursors of vaccine inequity such as high vaccine prices and vaccine delivery logistics have been hailed as a masterstroke toward improving global access to HPV vaccines especially in LMICs. At the heart of Gavi partnerships are its core members—WHO, United Nations Children Fund (UNICEF), World Bank, and Bill and Melinda Gates Foundation and other key development partners including governments, civil society organisations, vaccine manufacturers, research agencies, and other private sector players. Gavi achieved a historic agreement with vaccine manufacturers—GlaxoSmithKline and Merck to reduce the price of the bivalent (cervarix) and quadrivalent (gardasil) HPV vaccines which can cost more than $100 in High Income Countries (HICs) to less than $5 for Gavi-eligible countries where cervical cancer burden is the highest.
Despite such historic agreements, it has been argued that the price is still high and not sustainable for LMICs including Nigeria within the context of pervasive poverty, overstretched health budgets, and competing needs for scarce resources.
Beyond the agreement to make HPV vaccine affordable for target LMICs, Gavi provides significant funding and technical support for eligible countries that indicate interest to introduce HPV vaccines via two pathways – one for the national introduction of HPV vaccines and the other as a demonstration programme.
Before the introduction of free HPV in October 2023, HPV vaccines were sparsely provided in private and public health facilities at an average cost of $13, which is expensive considering the high poverty levels in the country and further impedes access for individuals who need them the most but cannot afford it.
Although low awareness of HPV and HPV vaccines has been reported among parents of Nigerian girls as barriers to vaccinating their kids, their willingness to vaccinate their daughters is high. Similarly, evidence from a pilot school-based HPV vaccination programme revealed the high acceptability of HPV vaccines among parents and adolescent girls in Nigeria. Such a high level of willingness and acceptability of HPV vaccines further strengthens the rationale for the national introduction of HPV vaccines in Nigeria.
President, Pediatric Association of Nigeria (PAN), Prof Ekanem Ekure, observed that HPV is the cause of several diseases, which include but are not limited to cervical cancer, genital warts, oropharyngeal cancer, penile and anal cancer.
According to her, “Its prevalence varies from place to place but data is limited in Nigeria. In a recent study conducted among women in Lagos a prevalence of 81per cent was reported whereas other studies have shown prevalence rates ranging between 10 and 35 per cent from other states. There are many serotypes of the HPV however serotypes 16 and 18 are responsible for almost 70per cent of cervical cancers in Nigeria.
“In Nigeria, it is estimated that about 12,000 cases of cervical cancer are diagnosed yearly with about 8,000 deaths yearly. These estimates are considered to be the tip of the iceberg because of the fragile and undeveloped level of our record keeping and statistics as well as limited diagnostic capacity and poor health seeking behavior of our population.”
Speaking on the primary challenges hindering widespread HPV vaccination adoption, she told The Guardian, “Rumours and misinformation affect HPV vaccine uptake. Lack of trust in the government has also contributed to the vaccine hesitancy that has been exhibited in various parts of the country. In addition to this inadequate stakeholder engagement in the background of intense activity of anti-vaccination groups resulted in suboptimal uptake in some parts of the country.”
MEANWHILE, the Federal Government had earlier in the year said Nigeria has attained 78 per cent of the 80 per cent national target for the HPV vaccination set for the pilot states where the vaccine was rolled out.
Immunisation Officer, Rivers State Primary Health Care Management Board, Joseph Urang, disclosed this in Port Harcourt, the Rivers State capital, during a two-day media dialogue on ‘Care for Small and Sick New-Borns, Oxygen Availability and the Introduction of HPV Vaccine in Nigeria.’
According to him, some weeks after the first phase of the vaccine rolled out on October 12 in 14 states and FCT, the Federal Government secured over six million doses of the HPV vaccine to protect girls aged nine to 14 years against cervical cancer and related diseases.
Urang said Taraba had the highest vaccination rate of 98 per cent, while Lagos had the lowest rate at 31 per cent. “There are over 170 types of viruses, with 12 currently classified as carcinogenic. HPV infects the basal keratinocytes of genital mucosa, oral mucosa and the skin, predominantly spread through sexual contact,” he said.
He added that long-lasting infection with certain types of HPV was the main cause of cervical cancer. About 3.5 per cent of women in the general population were estimated to harbour cervical HPV-16/18 infection at a given time, while 66.9 per cent of invasive cervical cancers were attributed to HPVs 16 or 18.
Urang, who emphasised that there were no known adverse effects following immunisation. He, therefore, urged parents and guardians to allow their daughters to take the HPV vaccine, saying “the vaccine is free, safe and potent against the virus. The perfect time to take the vaccine is between nine and 14 years of age, as it is most potent.”
Omigbodun added that policymakers and healthcare professionals need to work together to develop effective tools to educate community leaders and the general population about the benefits of cervical cancer prevention through HPV vaccination of pre-pubertal girls and cervical cancer screening for all women yet to attain the age of 65 years.